When you or someone you love struggles with Obsessive-Compulsive Disorder (OCD), it affects the entire family. It's not just about the person who has OCD; it's about how everyone close to them adjusts and responds to their condition.
Family accommodation in OCD is the process where family members modify their behavior to help a relative avoid anxiety and distress caused by their obsessions and compulsions. These changes can range from taking on additional responsibilities to assisting with rituals or reassurance seeking.
While these accommodations are made from a place of love and support, they can have complex effects on both the individual with OCD and the family dynamics.
What is OCD?
If you've ever felt the urge to double-check that you've locked the door or turned off the stove, you have a tiny glimpse into the lives of those with Obsessive-Compulsive Disorder (OCD).
But for someone with OCD, these urges don't stop with a quick double-check. They feel a strong need to perform certain actions over and over again. These actions, known as compulsions, are their way of trying to ease the stress from unwanted thoughts, or obsessions.
OCD is a type of anxiety disorder. There is a similar but different personality disorder called "Obsessive Compulsive Personality Disorder," (OCPD) but it requires different treatment than OCD. The treatment outcome will be based on a proper diagnosis.
OCD is like a broken alarm system. It tricks the mind into thinking there’s danger when everything is actually okay.
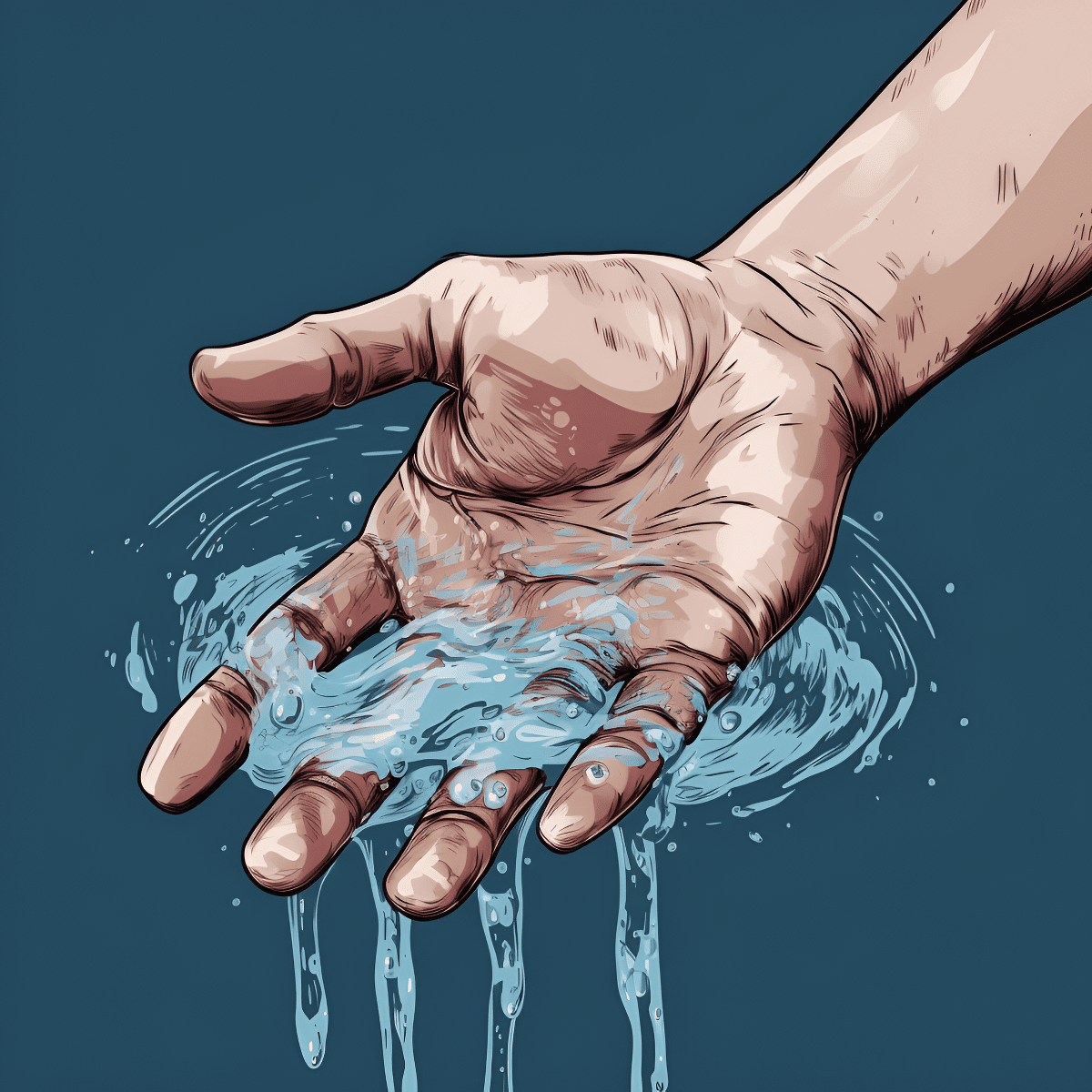
For example, imagine if your brain constantly told you that you needed to wash your hands to avoid getting sick, even if you had just washed them a minute ago. That's how it can be for someone with OCD—they're stuck in a loop of thoughts and actions that they can't easily get out of.
As you learn about OCD, you might come across terms like rituals and triggers.
Rituals are the compulsive behaviors a person with OCD feels they must do, like counting to a certain number or arranging items in a specific way.
Triggers are situations or items that bring on the obsessions and the need to perform rituals.
The estimated lifetime prevalence rate of Obsessive-Compulsive Disorder (OCD) is generally thought to be about 2-3% in the general population. This rate indicates the proportion of individuals in the population who are expected to experience OCD at any point in their lives.
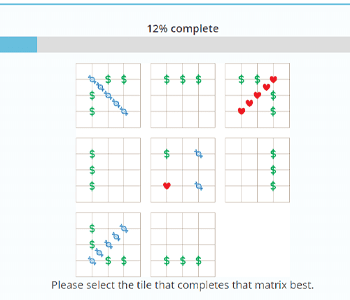
According to the Diagnostic and Statistical Manual (DSM-5) by the American Psychiatric Association, which is the handbook used by health care professionals in much of the world as the authoritative guide to the diagnosis of mental disorders, OCD has certain criteria that must be met for a diagnosis.
Firstly, a person must have obsessions, compulsions, or both. Let's break these down:
- Obsessions are repeated thoughts, urges, or mental images that cause anxiety. Think of them as unwanted guests in your mind, showing up without an invite and refusing to leave. These aren't just everyday worries about real-life problems; they're intense and often focus on themes like fear of germs, a need for order, or aggressive thoughts towards others or oneself.
- Compulsions are repetitive behaviors that a person with OCD feels the urge to do in response to an obsessive thought. It's their attempt to reduce anxiety or prevent something bad from happening. However, these actions are not connected in a realistic way with what they are designed to prevent or are clearly excessive. For example, washing your hands is a common response to the thought of germs, but in OCD, a person might wash their hands so many times that they become raw.
The DSM-5 specifies that these obsessions and compulsions must be time-consuming (taking up more than one hour per day) or cause significant distress or problems in social, work, or other important areas of functioning.
Another key point is that the obsessive-compulsive symptoms are not due to the physiological effects of a substance, like a drug or medication, and are not better explained by another mental disorder.
This means that a doctor would rule out other reasons for these thoughts and behaviors before diagnosing someone with OCD. The OCD symptom severity will be different for each patient, and the family functioning will be different depending on the severity.
Finally, a person with OCD might have insight into their disorder, meaning they understand that their OCD thoughts are not true. They might also have poor or absent insight, meaning they truly believe in their obsessions.
In some cases, this can reach the point of delusion, where their belief in the false ideas is unshakeable, despite clear evidence against them.
Adolescent psychiatry will approach treatment for pediatric OCD differently than adult OCD patients. The family's accommodating behaviors will also be different if it is a child versus an adult. Not to mention the family involvement will be far greater in everyday life, and it's important to support parents too.
What does Family Accommodation Mean?
In the journey of understanding OCD, you'll find that it's not a solo trip. It involves those closest to the person with OCD, often their family. Here's where we come to a critical term: family accommodation.
This isn't about booking a hotel room for a family vacation; it's about how family members change their own behaviors in response to a loved one's OCD symptoms and behavior management.
Family accommodation in OCD is when you, as a family member, might help or join in on the compulsions.
Let's say your brother has a compulsion to check the locks on doors multiple times before feeling secure. If you start checking the locks for him to ease his anxiety, that's family accommodation.
You're trying to help, but it's a bit like putting a band-aid on a leaky pipe—it might seem like a fix, but the underlying issue is still there.
This accommodation comes from a good place—you want to relieve your loved one's distress. Yet, over time, this can actually make the OCD stronger.
Think of it like feeding a small, demanding monster. The more you feed it, the bigger and more demanding it gets. So, while it might seem like you're doing the right thing in the short term, in the long run, you could be unintentionally helping the OCD to grow.
Adult patients will have different family involvement than those who experience OCD at an early age. Parental involvement in particular can have a massive impact on treatment outcome. The family routine is also really important for helping overcome compulsive rituals.
That's also why family based treatment is really important. OCD affects other family members too, not just the person with the disease.
Family focused treatments targeting family accommodation is especially important to avoid more severe OCD symptoms from developing. Cognitive behavior therapy can help with this, which we'll talk about more below.
The History of Family Accommodation in OCD Treatment
The concept of family intervention and accommodation in OCD isn't new, but it has gained more attention over the years. In the past, the focus was mainly on the individual with OCD, their inner world, and their behavior. Therapists worked one-on-one with patients, while families often waited in the dark, uncertain about how to help.
It wasn't until researchers like Tamar Chansky and Edna Foa started to look closer at the role families play that things began to change.
In the late 20th century, they observed how family members' reactions to OCD behaviors could affect treatment outcomes. If family members were accommodating too much, it could make the person with OCD less likely to learn how to manage their own symptoms.
Imagine if every time you were scared of a spider, someone else came in and removed it for you. You would feel relief, right? But what happens when you're alone with the spider?
That's the question therapists started to ask. They saw that without learning to face their fears, people with OCD might rely too heavily on others, just like relying on someone else to deal with the spider.
By the 1990s and early 2000s, studies were showing that involving families in treatment could lead to better results. Family-based therapies, like the PANDAS model (Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections), began to recognize the importance of teaching families about OCD and how to respond to it effectively.
As we moved into the 21st century, family accommodation became a key focus in OCD treatment. Therapy programs started to include families in their plans. They offered education and strategies to reduce accommodation, strengthening the person with OCD to face their challenges more independently.
Case Studies: PANDAS Model
Within the history of family accommodation in OCD, the PANDAS model stands out. PANDAS is an acronym for Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections. This model specifically looks at a subset of children with OCD where symptoms suddenly worsen following a strep throat infection.
This is called "Pediatric Obsessive Compulsive Disorder."
The idea behind PANDAS is that the strep infection triggers a misdirected immune response that results in inflammation in a child's brain. This inflammation can lead to a quick onset of OCD behaviors and tics, which are sudden, brief movements or sounds that the child can't control.
What does this mean for family accommodation?
Well, if a child develops OCD as part of PANDAS, their family might suddenly find themselves in the middle of a storm of compulsions and rituals. This can be overwhelming and confusing. Without understanding the connection to the strep infection, many parents of children might inadvertently start accommodating these behaviors, not realizing they are linked to a treatable medical condition.
By recognizing the signs of PANDAS early, which often include not just OCD symptoms but also other dramatic behavioral changes like mood swings, sleep disturbances, and urinary issues, families can seek medical intervention.
In other words, the child's OCD symptoms are only part of their symptoms. Adult OCD patients wouldn't have all the same signs.
Treatment typically involves antibiotics to address the strep infection and may also include other medications to control inflammation in the brain.
The PANDAS model has shed light on the fact that OCD can sometimes have a biological trigger, which can change the approach to treatment and the role of family accommodation.
It's a clear example of why understanding the underlying causes of OCD symptoms is crucial for providing the right support and avoiding unintentional reinforcement of the disorder through family accommodation.
Recognizing Family Accommodation
To truly understand and support a loved one with OCD, it's vital to recognize when and how you might be accommodating their compulsions.
Think of OCD as a pattern that your family member feels stuck in, like walking the same path every day because they believe the others are blocked or dangerous.
Recognizing these signs is crucial because it shows you where the boundaries have blurred between support and accommodation. Understanding this difference is the first step in helping your loved one build resilience against OCD.
By slowly pulling back on these accommodations, you encourage them to face their fears, much like teaching someone to swim by gradually moving away, letting them find their own strokes and pace.
Sign 1: Participating in Rituals
You might find yourself drawn into their rituals, such as checking locks or appliances, even if you know it's unnecessary. It’s like you’re both actors in a play, repeating the same scene again and again because they believe it's the only way to keep everyone safe.
Sign 2: Providing Reassurance
Another sign is offering constant reassurance. This is when your loved one asks for confirmation that everything will be okay, and you respond with comfort, maybe dozens of times a day. It’s similar to continually checking the weather forecast before stepping outside, even when you can see it’s sunny.
Sign 3: Avoidance Behaviors
You might also start avoiding things that trigger your family member's OCD. If they fear contamination, you might stop inviting guests over, or if they have fears about certain places, you may no longer visit these spots. It's like changing your route home to avoid a road they think is unlucky.
Sign 4: Taking Over Responsibilities
Finally, you could be taking on more chores or responsibilities to prevent their anxiety from spiking. If their rituals leave no room for household tasks, you might step in to fill the gap, much like covering for a co-worker who's out sick, except it happens every day.
Strategies for Reducing Family Accommodation

When you start noticing the signs of family accommodation in your life, it's time to learn strategies to gently reduce these patterns.
Changing the way you respond to your loved one's OCD can be challenging, but it's also a path toward greater independence for them and healthier dynamics for the whole family.
Reducing family accommodation doesn't mean pulling away support. It's about shifting the kind of support you provide—from one that inadvertently maintains OCD to one that empowers your loved one to combat their disorder.
Strategy 1: Setting Gradual Boundaries
Begin by setting small, manageable boundaries. For instance, if you usually give in to checking the stove multiple times a night at your loved one's request, you might decide to reduce this to just once before bed.
Strategy 2: Encouraging Self-Reliance
Encourage your family member to start facing their fears without your involvement. This could mean supporting them to resist a compulsion or to wait longer before giving in to it.
It's similar to watching a child ride a bike without training wheels for the first time; they might wobble, but they need to feel that wobble to learn balance.
Strategy 3: Communication
Open and honest communication is key. Have a conversation about the changes you're making and why. It's not unlike navigating a dark room together; you need to talk about where you're going so you don't bump into things—or each other.
Strategy 4: Educating the Family
Educate everyone in the family about OCD and family accommodation. Knowledge is a powerful tool—it helps you understand the landscape and find your way through it.
Strategy 5: Seek Professional Guidance
Lastly, consider seeking the help of a therapist trained in OCD and family systems. They can be a guide, offering strategies and encouragement while helping you track progress and adjust your approach as needed.
Offering Support Without Accommodating OCD
Creating a supportive environment for a loved one with OCD means fostering a space where they can confront their fears safely and constructively, without depending on rituals or accommodations.
By nurturing an environment that values effort over perfection and progress over immediate results, you help your loved one build the resilience and skills they need to manage OCD.
This doesn't mean ignoring their struggles; it's about changing the support you provide from one that holds their hand at every step to one that cheers them on as they learn to walk the path independently.
Strategy 1: Positive Reinforcement
When your family member resists a compulsion or takes a step towards managing their OCD independently, acknowledge their effort.
Positive reinforcement is like sunlight to a plant; it encourages growth. A simple "I'm proud of you for waiting five more minutes before washing your hands" can be incredibly affirming.
Strategy 2: Establish Routines
Establishing regular routines can provide a sense of predictability and control, which can reduce the perceived need for compulsions.
This is like having a reliable schedule for a school day; knowing what to expect can ease anxiety and make the day go smoother.
Strategy 3: Stress Reduction Techniques
Teach and practice stress reduction techniques together. Whether it's deep breathing, mindfulness, or exercise, these are tools they can use instead of compulsions to manage anxiety disorders.
Strategy 4: Collaborate on Problem-Solving
Encourage collaborative problem-solving when OCD-related issues arise. This means sitting down together and brainstorming ways to handle a trigger.
Strategy 5: Focus on Overall Well-being
Don't just focus on OCD—encourage activities that promote overall well-being. Whether it's hobbies, social outings, or family time, these experiences can enrich your loved one's life and reduce the overall focus on OCD.
Treatment and Family Accommodation

When it comes to overcoming OCD and the challenges of family accommodation, professional treatment often plays a critical role.
Professional treatment for OCD is not just about managing symptoms; it's about changing the underlying dynamics that sustain the disorder. It empowers both the individual with OCD and their family to transform their interactions into ones that promote healing and growth.
With the right help, families can learn to stop accommodating OCD in a way that's compassionate and constructive, eventually leading to a more balanced and fulfilling life for everyone involved.
Strategy 1: Cognitive-Behavioral Therapy (CBT)
One of the most effective treatments for OCD is Cognitive Behavioral Therapy (CBT), specifically a type called Exposure and Response Prevention (ERP). In ERP, a therapist helps the person with OCD face their fears without giving in to compulsions.
Strategy 2: Family Therapy
Family therapy can also be valuable. In these sessions, families learn how their interactions and behaviors might contribute to the OCD cycle, and they develop strategies to change these patterns. It's akin to a team learning new plays to improve their game.
Strategy 3: Medication
Sometimes, medication is recommended to help manage OCD symptoms. Medications like SSRIs (Selective Serotonin Reuptake Inhibitors) can reduce the anxiety that fuels OCD, making it easier to engage in therapy. Think of it as wearing a life jacket when you're learning to swim—it doesn't swim for you, but it provides support as you learn.
Strategy 4: Education and Training
Professionals can also provide education and training to families about OCD and how to handle symptoms. This knowledge is a powerful tool—like a manual for complex machinery, it helps you understand how it works and how to use it effectively.
Strategy 5: Support Groups
Finally, support groups for families can be a source of comfort and advice. Sharing experiences with others who understand can be as relieving as finding shelter in a storm; you realize you're not alone, and you can learn from those who've been through it before.
Frequently Asked Questions (FAQs)
1) What exactly is family accommodation in OCD?
Family accommodation in OCD refers to the actions or behaviors that family members might perform to help a loved one avoid distress related to their obsessive-compulsive symptoms. This can range from participating in the rituals to helping avoid certain triggers.
2) Why do families accommodate OCD behaviors?
Families often accommodate out of love and a desire to reduce their loved one's distress. It's a natural response to want to help someone you care about, but over time, this can reinforce the OCD behaviors.
3) How can I tell if I'm accommodating my family member's OCD?
Look for signs like modifying family routines, providing reassurance, or assisting with rituals. If your daily life is changing to prevent anxiety for someone with OCD, you might be accommodating their behaviors.
4) Is family accommodation harmful in the long term?
While accommodation may reduce anxiety in the short term, it can reinforce the OCD over time, making the disorder more entrenched. It's important to find a balance between supporting your loved one and not reinforcing their OCD behaviors.
5) Can reducing family accommodation cure OCD?
Reducing accommodation alone won't cure OCD, but it's a significant step towards managing the disorder effectively. It should be part of a comprehensive treatment plan that may include therapy, medication, and support.
6) What should I do instead of accommodating OCD behaviors?
Focus on supportive strategies that encourage independence and resilience in the person with OCD. This can include reinforcing non-OCD behaviors, maintaining a supportive environment, and seeking professional help.
7) Will my loved one get upset if I stop accommodating their OCD?
It's possible that they might feel more anxious or upset initially, as the safety net of accommodation is being removed. However, with proper support and professional guidance, they can learn to manage their anxiety in healthier ways.
8) How do I start the conversation about reducing accommodation?
Approach the topic with empathy and understanding. Communicate your desire to support them in a way that's helpful for their long-term well-being. It might be beneficial to have this conversation with a therapist present.
9) Are there any risks to stopping accommodation abruptly?
Abrupt changes can be very stressful for someone with OCD. It's usually recommended to reduce accommodations gradually, with professional guidance, to ensure the person with OCD can adapt and develop coping skills.
10) Where can I find support for myself as I help my family member with OCD?
Support can come from many sources, including therapists who specialize in OCD, support groups for families of individuals with OCD, and online resources that provide information and community connections.
Conclusion
In navigating the complexities of OCD, understanding and addressing family accommodation is crucial.
Remember, while it can be challenging to change the patterns of accommodation, doing so is a powerful step toward supporting your loved one's recovery.
Professional help, consistent strategies, and a compassionate approach are your tools in this process. As you move forward, remember that setbacks are not roadblocks but signs along the way, guiding you to adjust your path as needed.